Blog
Wellsteps accomplished the impossible: they got stupider.
Readers of Why Nobody Believes the Numbers may recall that you can’t reduce a number by more than 100%. This is true no matter how hard you try. And just in case our friends Down Under were wondering, this is not one of those things that’s the opposite in the Southern Hemisphere.
Wellsteps is giving that assertion a run for its money.
Following that headline above (from a full-page spread in the Boston Globe) they’ve doubled down on stupidity to win the wellness industry’s race to the bottom, and, with the demise of Interactive Health, Wellsteps is easily the dumbest vendor in all of wellness.
Still, you have to admire their commitment to stupidity. I and others have pointed out maybe a dozen times that their entire business doesn’t accomplish anything other than harming employees, but they refuse to budge.
Calling them the dumbest vendor in all of wellness is quite a compliment. That’s because the alternative would be to call them the most dishonest vendor in all of wellness. Besides insulting their integrity, that’s not an easy feat to accomplish in this industry. It would be like calling out a specific entitled zillionaire as the most dishonest parent in the entire Varsity Blues scandal.
Perhaps disheartened by their loss of the uncoveted Deplorables Award to Angioscreen after having won or shared two of the last three, they have decided to take stupidity to a new plateau.
Their “Updated ROI Calculator”
The reason they’ve made the news today is that they’ve just published an “updated ROI calculator.” And a big thank you to Jon Robison for forwarding it to me, as Wellsteps has banned me from their linkedin group and everything else.
There are a few things you might want to know about their updated ROI calculator. As you’ll see once you expose it to light, this updated ROi calculator:
- is not “updated“
- doesn’t show an ROI
- doesn’t calculate.
Three lies in three words. That breaks Ron Goetzel’s record of 14 lies in 45 minutes.
No need to take our word for any of this. Here’s the only thing that is updated: the font. This makes it easier to see what happens if you actually try to enter data into this model. Sort of like actually trying to drive a Yugo
Start by zeroing out inflation as a confounder (“0”). Then, for simplicity and consistency, enter “1” into number of employees, as below. I entered $1000 into annual healthcare costs, just to use a round number.
Then let the games begin.
Let’s see how much they save in the best-case scenario. Enter 100% into the two fields “% Employees that [sic] are obese” and “% Employees that [sic] are smokers.”
As an aside, normally one would use “who” in this situation, but they don’t, for two reasons. First, One of Wellsteps’ signature moves is creative sentence structure, spelling, and mixed metaphors. The CEO, Dr. Steve Aldana, called the late award-winning journalist Sharon Begley a “lier.” He once accused me of violating the Law of Conservation of Matter, saying that I am “great at creating BS out of thin air.”
Second, perhaps the reason they preferred “employees that” to “employees who” is because another of their signature moves is to dehumanize employees. Their exact words, subsequently deleted after criticism, were: “It’s fun to get fat. It’s fun to be lazy.”
Back to the Calculator
Let’s see what happens if you do a fantastic job, and reduce the number of “employees that are obese” and “employees that are smokers” from 100% to 0%. So enter those two figures:
Then go to the right — directly on top of this “hockey stick” graph as you can see, and hit “savings from wellness programs.”
Congratulations. You’ve reduced the $1000 spend by $1379, which is a reduction of more than 100%. While I merely allegedly violated the Law of Conservation of Matter, they’ve just clearly violated a basic law of arithmetic, and those are strictly enforced.
You might say: “That’s not fair. Let’s use a more realistic risk reduction figure, like 0%, which is what all the literature says is achieved:
In the immortal words of the great philosopher Gomer Pyle: “Surprise, surprise, surprise.” You still show mathematicaly impossible savings.
You still show savings even if employees get worse. This is Wellsteps’ signature move in real life, as they harmed the employees at the Boise School district…and still fabricated massive savings:
The actual savings they fabricated — along with their inadvertent admission that costs actually increased — can be found here. Costs can’t go up and down at the same time. Yet another rule of math that is strictly enforced.
What if you don’t have any employees on your health plan, so you spend $0 to begin with? Turns out you can still save a bundle if you have no costs to begin with, even without reducing smoking or obesity.
Before you start fiddling with it, be aware that the very stable geniuses at Wellsteps who came up with this calculator once accused me of “entering false data” into it. So make sure your “data” isn’t “false.” To avoid that:
- use only arabic numerals…
- …in base ten.
Turns out no matter what data you enter, you save money. Don’t take my word for it–see it with your own eyes.
Stupid? Well, let’s just put it this way. NASA engineers need not worry about their job security on account of Wellsteps, because these people are not rocket scientists.
Or Wellsteps’ CEO, Steve Aldana, actually dishonest?
Let’s examine the evidence both ways. Here are the three best arguments for stupid:
- He says he needed 11 years to get through college. (p. 7) That’s 4 more years than Bluto Blutarski.
- He thinks “even one more bite of a banana” will improve your health.
- He is friends with Ron Goetzel.
Here are the the three best arguments for dishonest:
- He admitted that his alleged savings at the Boise School District was just regression to the mean. (Scroll down.)
- He knows this “model” is fabricated and has criticized me for pointing that out.
- He is friends with Ron Goetzel.
And let’s not forget that Wellsteps’ claim to fame is actually bragging about harming employees. To this day, they are the only vendor willing to publish data admitting that employees got worse on their watch. And that puts them in a category all their own. Like Juan Garcia, whose espionage work won him the highest military awards from both Germany and Britain, this performance earned them both a Koop Award (see #3 above) and a Deplorables Award.
Does that mean they are dishonest, stupid, or both? To slightly paraphrase the immortal words of the great philosopher Clarice Starling, there isn’t a word for what they are.
Update: Many of you know about the $3 million reward for showing wellness works. If Steve Aldana and his team of very stable geniuses with very good brains can show that their calculator is more accurate than Quizzify’s ROI calculator, I am doubling my $3 million reward and halving the $300,000 entry fee. The rest of you can stop reading here. Steve, that would be a $6 million reward for a mere $150,000 entry fee.
“New” EEOC wellness incentive rules now DOA!
Within minutes of Quizzify’s blast email predicting that the EEOC’s rules released two weeks ago would be DOA, it is now a lock that they are toast. The White House made two announcements last week confirming this:
- They froze all non-emergency Notices of Proposed Rulemakings (not a misprint — two plurals)
- They rejiggered the EEOC, promoting the two pro-employee Commissioners to the Chairmanship and Vice Chairmanship.
This means the huge loophole in the announced rules, allowing most outcomes-based wellness programs, will be closed.
Is this an existential threat to the wellness industry? At first glance, it would seem to be. But you can join our webinar to learn so this existential lemon can be turned into existential lemonade.
Leading wellness attorney Barbara Zabawa and I are hosting a webinar on this topic on Monday, February 1st, 1:00 EST. You can register here (and get access to the recording and slides as well.) Focus will be on how to ignore the new rules, and maintain your program as is. Yep, just like with surprise bills, we’ve figured out how to game the system.
The EEOC has just released their rules for clinically based wellness programs.This step is called the “Notice of Proposed Rulemaking,” or NPRM, to be published in the Federal Register’s mellifluously named Notices of Proposed Rulemakings for public comment. “Public comment” is code for “the perps with the most to lose will flood the thread with disinformation.” Expect the US Chamber of Commerce, the vendors and Ron Goetzel and his cronies to weigh in heavily, each more shamelessly than the next. They have a lot of (your) money at stake here.
When NPRMs are posted for public comments, you know who never makes public comments? The public. So it’s up to you and me to pick up the slack, and point out that these perps have no clothes. Feel free to grab posts from TSW to add to the comments.
And the envelope please…
Most importantly, incentives for participation-based programs need to be cut back to “de minimis.” And, unlike when the rules were first floated (and true to the intent of the judge who found that forced wellness programs were not voluntary), de minimis has been defined. It looks like the IRS definition — water bottles, t-shirts, small-denomination gift cards. I had thought perhaps $200 would be OK. That is clearly outside the realm of de minimis. That could change if the perps flood the comments.
My own opinion: it is perfectly ok, even desirable, for organizations to offer employees screening. Just don’t make them do it. I myself voluntarily get my Hb a1c screened every year, to make sure I’m playing enough ultimate frisbee to offset my consumption of LA Burdick’s insanely good chocolate.
And it is perfectly OK to educate employees on why they should want to get screened (or, in the case of younger, healther employees, why they shouldn’t). Screening would then be truly voluntary.
However, many organizations want to maintain their current participation-based programs with their current incentives or penalties…and many vendors want to keep their revenues intact.
For these groups, Barbara and I are offering this webinar, to show how to do exactly that.
So far, so good, but…
That was all about participation-based programs. Health-contingent, or outcomes-based, programs are a different story altogether. The EEOC is basically pro-employer these days. So they have figured out how to circumvent the spirit of Judge Bates’ December 2017 decision vacating the old rules in which forced programs were defined as “voluntary,” without violating the letter of his decision. But this massive loopholecould circumvent the ruling only for outcomes-based programs, not participatory ones.
This loophole allows you to continue to be able to subject employees to fines of thousands of dollars in outcomes-based programs. Most employees hate being forced to submit to these programs (“I’d like to punch them in the face,” said one), and they invariably lose money. However, the losses in program fees and employee morale — all admitted by the wellness industry trade association — is more than offset by the “immediate employer cost savings,” as Bravo puts it, generated by collecting the penalties from employees who refuse to let unlicensed wellness vendors play doctor.
However, most outcomes-based programs, while arguably complying with these new rules under the Americans with Disabilities Act, violate the Affordable Care Act. With the well-documented, Validation Institute-validated exception of US Preventive Medicine, they invariably fall short of the ACA’s standard of being “reasonably designed to reduce risk or prevent disease.” That hurdle was set low enough to allow even the worst outcomes-based wellness vendors to clear it, and yet they don’t. They violate guidelines with impunity, forcing employees to undergo tests that no doctor would ever order and that get D ratings from the US Preventive Services Task Force (USPSTF).
Just too many epic fails, all documented for the last five years on this blog and sometimes in the media, including Koop award winners like Wellsteps, arguably the industry’s worst program now that Interactive Health has gone bankrupt. Ironically, Wellsteps is also among the best-documented programs. Why they insisted on publishing their own self-immolation is anyone’s guess. No one can argue that programs violating the USPSTF guidelines and, as we’ll see, harming employees, could possibly be considered “reasonably designed to prevent disease.”
This is not just about the money.
Outcomes-based programs can and do harm employees. Sometimes wellness vendors — I’m looking at you, Wellsteps — even admit their harms.
Yale employees sued Yale, for example, due to the psychological and physical harms of their program. One Yale breast cancer survivor was almost forced into getting a mammogram, even though she had already undergone a double mastectomy. Had it not been for Yale’s union and the AARP’s support, she would have been fined $1250.
TSW has published many stories of harms, summarized here. Not to mention what happens when you fine your employees for not losing weight. Guess what — they respond in very predictable fashion, packing on the pounds before the weigh-in and then crash-dieting to take them off. And our #1 most-searched phrase? “How to cheat in a corporate wellness program.” https://dismgmt.wordpress.com/2019/01/07/breaking-shocking-news-employees-cheat-in-wellness/
Still, if you insist on keeping an outcomes-based program, the “hack” we’ve figured out of the new regs applies to outcomes-based programs as well. Seriously.
So if you have a program (and very few people with outcomes-based programs read this blog, or else they would have already dropped them), you’ll want to attend the webinar to figure out how to preserve it. And if you don’t have a program, you’ll want to attend just to understand what the EEOC tried to do with this massive loophole and how we got the better of them.
Answer Leapfrog’s 20th Birthday Trivia Question to win $100
Dear They Said What Nation,
To celebrate Leapfrog’s 20th Birthday Week, Leah Binder posted 3 questions in our chat on Linkedin. One of the 3 remains unanswered…and I am personally upping the ante to $100 for the first correct answer!
So have at it. Here is a hint: this person was an overnight sensation before become the person with the most things un-named for him. The full question is in the interview.
Once again, Hppy 20th Birthday to Leapfrog!
Dear They Said What Nation,
Happy 20th Anniversary to The Leapfrog Group. In 20 years they have become arguably the most untainted healthcare not-for-profit in DC. It’s not easy to stay untainted for 20 years, but they have. By contrast, providers, PBMs and vendors “sponsor” other groups, and — get ready — the other groups advance their agendas instead of consumers and employers. Simply doesn’t happen with Leapfrog.
Even though it’s their birthday, you’re the ones getting the presents. Yes, members of TSW Nation can actually win prizes. Not for blowing the whistle on dishonest wellness vendors (though that too), but rather by answering a couple of general interest trivia questions right. If someone does the Mary Wells thing and guesses ahead of you, you can still at least be entered in a runner-up drawing
As of this writing, there are no correct answers yet…though everyone has heard of the two people and you’ll kick yourself for not guessing right.
Once again, here is the link. No time to waste, as the deadline is 4 PM today.
I was caught making stuff up…again!
In the immortal words of the great philosopher Britney Spears: “Oops, I did it again.”
Another mistake caught! This time by the esteemed Scott Breidbart MD. I had written that the incidence of colon cancer in the 45-to-49-year-old population was 0.007%, having misread my own posting. I confused the total <50 incidence with the 45-to-49-year-old incidence, which is a whopping 0.035%, as Scott said.
I had cited the wrong number when Scott and I got into a kerfuffle about whether 45-to-49-year-olds should be screened for colon cancer. That is the new USPSTF guideline. Honestly, even at 0.035%, I still wouldn’t recommend that employers get involved in this decision. Here’s a wacky idea: let’s leave this one to the patient and the doctor! Oh, I know it sounds crazy but it just might work.
My logic would be that many folks in that 0.035% would already have had symptoms. So the percent findable with a screen is somewhat less than that. Further, the complication rate from colonoscopies exceeds 0.035% by at least one decimal point. Not to mention that, surely, as an employer, you can find better ways to spend your money.
Scott would say, quite correctly, that you don’t have to get screened using a colonoscopy. Cologuard and FIT testing are completely non-invasive. I myself recently did Cologuard. As instructed on the box, I took my “sample” to the local UPS store to mail back and as coincidence would have it, someone else was in the store doing the same thing. Maybe this is catching on, because the UPS rep said he was shipping a fair number of Cologuard samples these days. (Sidebar: as far as I’m concerned, UPS can’t pay these guys enough.)
I would then observe back to Scott that many non-Quizzify users don’t know about alternatives to colonoscopies, and (like with Silver Diamine Fluoride for cavities), the providers aren’t telling them, in order to protect their revenues. If you really want to get down and dirty on this topic, so to speak, here is the Quizzify writeup.
Still, we don’t go against the USPSTF. Color us neutral even though our gut, so to speak, says the opposite. As far as this decision is concerned, I’d say let’s leave it to the doctor and the employee.
Scott and I are in total agreement on that point and this next point. (I checked with him just now. I make enough enemies on purpose without making any accidentally.) Our advice to employers is, so to speak again, to butt out.
Or, for those who prefer visual mnemonics…
If anyone is keeping score at home, Part 1
This is the second mistake (or at least the second time I’ve been caught) in the last two years. At this rate, I will make 4 more mistakes during the 2020s, which will be a new record for me.
The leaders are tightly bunched for first place:
- Scott Breidbart – 1
- Keith McNeil – 1
- Tom Milan – 1
- Jeff Hogan – 1
- Entire wellness industry – 0
If anyone is keeping score at home (Part 2), here are the previous ones…
For the fourth time in as many decades, I’ve been caught! This is not to say that I’ve only made 4 miscues in the most recent 4 decades. Just that I’ve only been caught 4 times in these 4 decades. Not including the time I caught myself actually thinking disease management (DM) saves money. Until then, basically everything I said was a lie, however unintentional, because in my naivete I thought DM worked. Silly me.
Jeff Hogan joins the few, the proud, who have called me out for saying things that aren’t exactly accurate. I’m putting this blog on top of the previous one to make it easier to track my cumulative miscues, in case you’re keeping score at home.
In this case, he referenced a study in Health Affairs showing that bundled payments reduced the cost of surgeries by 11%. I saw that abstract and immediately assumed that, like many other bundled payments, the reason the cost per procedure declined is that the number of procedures increased, by surgeons adding more “easier” and hence less costly procedures. This would reduce the cost/procedure but total costs would increase due to more procedures.
I couldn’t link through to that study (nor can you, most likely) from that abstract, to test that hypothesis. But since it is Health Affairs I just assumed that their peer review for that article is as sloppy as it is for wellness articles. Ron Goetzel published a nonsensical article there, which, among other things, concluded that only about 5.5% of the cohort smoked because only 5.5% of the cohort admitted they smoked, on a risk assessment. Since the US smoking rate is more like 18%, the correct conclusion would have been that two-thirds of smokers lie on risk assessments. I would have caught that in peer review but Health Affairs allows authors to pick their own toadies as peer reviewers.
So, without actually reading the Health Affairs study, I assumed they applied the same lofty standard of peer review to this article as to Goetzel’s:
They don’t appear to have tracked the number of cases. A classic thing hospitals and doctors do when they get paid per case is to perform surgeries on people who may not have needed them. These people will have lower-than-average costs and complication rates…but be reimbursed the same.Or, in the immortal words of the great philosopher Claude Rains, “Owing to the seriousness of this crime I’ve instructed my men to round up twice the usual number of suspects.
Jeff wrote back:
Al: Did you read the same Health Affairs article that I did? The citations and case tracking is quite detailed in the report and appendix. Not only did they carefully examine the number of cases but they used some very intensive methodologies for doing disruption analysis.
He helpfully attached a pdf. It turned out they had indeed tracked the number of referrals not going to surgery, and almost a third did not, in fact, go to surgery. This factoid never made it into the abstract, but was buried in the article.
So kudos to Jeff and if he sticks around another 8 years, 9 months and 22 days, at my current pace, I’ll be due for another mistake.
Guilty as charged. Someone called me out on yet another mistake buried in my 500,000 words published to date.
Yep, the number of members in the most exclusive club in healthcare outcomes analysis just rose by 33%, as Tom Milam of TrueLifeCare joins Corey Colman and Keith McNeil in justifiably calling me out.*
To put this track record in perspective, Ron Goetzel has been caught 14 times. You might say, well, 14 isn’t that much different from 3 in absolute terms. (In percentage, it is, but we’ll let that slide.)
Except that I needed an entire decade to rack up 3, while Ron needed only 45 minutes to tally 14. Over the decade, his number would be more like approximately eleventy zillion. It depends how you count the ones where he doctored numbers that were phony to begin with and then doctored them back again to the original phony numbers, after insisting that the doctored numbers were real. If you’ve lost track on all the doctorings that I just now published a companion blog post on it.
So what was the mistake?
[SPOILER ALERT: The rest of this post is boring.]
It’s kind of anticlimactic, and quite obscure. By way of background, I routinely analyze wellness-senstive medical event (WSME) rate trends for large employers and health plans. It’s not rocket science, but it’s totally valid. Indeed, it’s the only population-based observational analysis that is valid. (RCTs are not observational. But you knew that.). It was even embraced by Ron Goetzel’s very own outfit: the Health Enhancement Research Organization — before they realized that valid measures are the wellness industry’s kryptonite.
The WSME tally is also the only observational methodology accepted by the Validation Institute for employers and health plans.
Here’s what the national WSME rate looks like. (I think there was a reporting or transcribing error by one of the reporting states in 2005-2006, to the extent anyone noticed the inflection in the graph, or cares.) This graph of WSMEs shows that, over the decade+ period of the greatest growth of workplace wellness, that there was no improvement in event rates relative to the US population that would not have had access to workplace wellness — Medicare, Medicaid and the uninsured. Obviously their raw rates were higher. This is a difference-of-differences analysis.
Quite the contrary, it appears that if anything the employer-insured cohort trended worse than the control.
Tallying this rate requires our data extraction algorithm to collect ER and IP events primary-coded both to the disease in question, or else are common complications of the disease in question. We pick common complications based on two factors:
- How likely is someone with the disease in question to get the complication?
- How likely is it that the complication in question occurs in someone with the disease?
Remember, we only tally primary codes because we want to simplify the analysis enough that we can be 100% sure of comparability between any given payor and other payors comprising the benchmark. So we look for an “80-20 rule” in what we include in the primary code data extraction.
Our diabetes rate includes quite a number of complications that fit that description., one of which is cellulitis. Diabetics are much more likely than non-diabetics to get cellulitis in their extremities — feet in particular — because they often can’t feel a cut. (Also the skin on their feet can be thinner than it should be.) Likewise, cellulitis of extremities is much more likely to be diagnosed in diabetics than non-diabetics.
If you can’t feel it, you won’t treat it. And therefore your odds of cellulitis in your foot are high. However, cellulitis in non-extremities would correlate much more loosely with diabetes, since diabetics can still feel and see skin issues elsewhere on their bodies. Therefore, not all cellulitis codes, by a longshot, are included in our analysis.
While we included cellulitis of the foot (and leg, also common enough), we somehow — despite having done these analyses 20 to 30 times a year for 15 years — omitted cellulitis of the toes. Sort of like the Matisse painting hanging upside down in the Museum of Modern Art for 47 days, no one else noticed either. Yet even the most intellectually challenged members of the wellness industry’s self-anointed awards committee understand the anatomical fact that, technically speaking, the toe is part of the foot.
Le Bateau, Henri Matisse
Honestly, when all is said and done, this won’t change anyone’s results much, and all the changes will be in the same direction vs. history (which is also going to be recoded) and vs. the benchmark/average, likewise recoded. This is especially true in the working-age population, which comprises most of our analysis. Nonetheless, kudos to Tom Milam for becoming the third member of this most exclusive club.
*Your chances of joining this club are quite remote, statisically speaking. They are even more remote if you didn’t notice the arithmetic error just now. n increase in membership from 2 to 3 is a 50% increase, not a 33% increase. And the painting is still upside down…
Official Rules for Acacia $100,000 Validity/Outcomes Challenge
Congratulations to Radial Health for achieving the highest level of validation from the Validation Institute. That comes with a $100,000 Credibility Guarantee.
In rare cases, such as Virta Health or Sera Prognostics or Ault International Medical Management, I add my own guarantee.
Any mental health vendor mentioned in the Peterson Report (I’m lookin’ at you, Lyra) can challenge my statement that Radial (nee Acacia) has the most validly measured good outcomes. Here are the terms to earn the $100,000.
Terms and Conditions of Challenge
Selection of Judges
There will be five judges, selected as follows:
- Each side gets to appoint one, drawn from the Healthcare Hackers listserve with 1000 people on it, from all walks of healthcare.
- Two others are appointed objectively. That will be whichever health services researchers/health economists are the most influential at the time the reward is claimed. “Most influential” will be measured by a formula: the highest ratio of Twitter followers/Twitter following, with a minimum of 15,000 followers.
- Those four judges will agree on the fifth.
Using the criteria below, judging will be based on validity of the measurement. Measurements deemed invalid, such as those described on the Validation Institute site, would be a disqualifying factor, i.e., any challenge by a vendor that is not validated by the Validation Institute.
If the challenging party/vendor is deemed by the judges to have an equally valid metric as Client, the decision is made on the impact of the program in outcomes for people with treatment-resistant OCD.
Written submissions
Each side submits up to 2,000 words and five graphs, supported by as many as 20 links; the material linked must pre-date this posting to discourage either side from creating linked material specifically for this contest.
Publicly available materials from the lay media or blogs or the Validation Institute may be used, as well as from any academic journal that is not open-access.
Each party may separately cite previous invalidating mistakes made by the other party that might speak to the credibility of the other party. (There is no limit on those.)
Oral arguments
The judges may rule solely on the basis of the written submissions. If not, the parties will convene online for a 2.5-hour recorded virtual presentation featuring 10-minute opening statements, in which as many as 10 slides are allowed. Time limits are:
- 30-minute cross-examinations with follow-up questions and no limitations on subject matter;
- 60 minutes in which judges control the agenda and may ask questions of either party based on either the oral or the written submissions;
- Five-minute closing statements.
Entry process
The entry process is:
- Challenger and TheySaidWhat deposit into escrow the amount each is at risk for ($100k for the Challenger, and $100k for TheySaidWhat). Each party forwards $10,000 to the judges as well, as an estimate of their combined fees and/or contributions to their designated nonprofits.
- If the Challenger or Service Provider pulls out after publicly announcing an application, the fee is three times the amount deposited.
- The escrow is distributed to the winner and the judges’ fees paid by the winner are returned by the judges to the winner, while the judges keep the losers’ fees.
Other
The competition is open to any mental health vendor outcomes claim which was made in the Peterson Report.
Aon giving Goetzel and Wellsteps a run for their money in the integrity department
The misstatements of the latter two have been well-documented in these pages. Simply search on either name, assuming your internet connection has enough “bars” to capture all the content
Lately Aon has been playing catchup. First with Accolade. Then Lyra. Then it got caught (I need to add “allegedly”) taking money from PBMs.
And now, they are claiming that weight loss drugs save money. Coincidentally, they offer a program (meaning take someone else’s program and mark it up) to “help” employers square this circle.
My “observations” on their arithmetic, such as it is, got picked up by The Health Care Blog, so i would encourage everyone to read them there.
Aon finally shows their hand. It’s in the cookie jar.
Aon’s claims of savings for the companies such as Lyra and Accolade that retain them to “show savings” appeared to be so obviously fabricated that I thought: “Wow, no actuary could possibly be this stupid and/or this dishonest.”
Then I saw they likely had their hand in the PBM cookie jar as well, allegedly collecting money from Express Scripts to steer Johnson & Johnson to them and not hiding it well enough to avoid being caught. So I thought, maybe they are this stupid and/or dishonest.
But before I actually came out and said: “Aon is stupid and/or dishonest,” I thought I should write to them and ask if perhaps I was the one who was missing something. So I wrote to them on Linkedin and asked to get back to me by Tuesday to correct any mistakes in those analyses linked above.
They apparently read those analyses and did not respond. Just to make sure they had every opportunity to correct any mistakes, I then wrote to their chief actuary on Linkedin on email on Tuesday to give them another extension:
GLP-1 Coverage: Dissuade the Curious and Educate the Serious
We are going to take time out from our usual policing of the perps in this field (and if you missed the last one, here it is) to show you something positive:
- you can cover weight loss drugs without breaking the bank
- while at the same time segmenting your population into those likely to fail and those likely to succeed on them
Yep, Quizzify’s Weight Loss Drug Companion Curriculum “dissuades the GLP-curious and educates the GLP-serious.” That is exactly what you want to do. After taking our 27-question Curb Their Enthusiasm introductory quiz covering the downsides of GLP-1s, only those who are very serious about improving their health will continue onto the drugs.
Here is a 5-minute read on how we do this, including our two favorite questions among those 27. If you took this quiz, would you want the drugs? I didn’t think so…
If you prefer the 3-minute version in video, try this https://www.youtube.com/watch?v=FeNQZGRpeNQ
Please put comments in Linkedin, as I now consolidate them all into one place. https://www.linkedin.com/posts/al-lewis-%F0%9F%87%BA%F0%9F%87%A6-57963_every-other-entity-involved-in-weight-loss-activity-7242511398851813376-1xOM?utm_source=share&utm_medium=member_desktop
Aon channels Britney Spears in Lyra report
An open (and also sent, received, read and unobjected to) letter to Aon’s chief actuary, Ron Ozminkowski.
Dear Mr. Ozminkowski,
It seems that there are always some rookie mistakes in your analyses. Either that, or you are simply “showing savings” because your clients are oxymoronically paying you as “independent actuaries” specifically to show savings. I will assume that your mistakes are just rookie mistakes, rather than deliberate misstatements. Yet as I recall, you never fixed your Accolade analysis after it was pointed out that your own assumptions, when correctly analyzed by someone whose IQ possesses that critical third digit, inexorably led to the opposite conclusion: Accolade loses money.
Perhaps that bug is a feature for your clients, and indeed your job description is to “show savings.” Mine is the opposite: to demonstrate integrity.
If I am wrong and you are genuinely trying to do the right thing, I would be happy to fly out there and teach you people how to do arithmetic, because, in the immortal words of the great philosopher Britney Speers, oops, you did it again. This time for Lyra. With all the money they paid you, it seems like they should be able to expect correct analysis. They might be very disappointed in you.
On the off-chance that you’d like to see what a real study design looks like in mental health, Acacia Clinics would be a good one to review. Here is the Validation Institute report and here is the science underpinning it.
If you are quite certain your arithmetic is correct despite all indications to the contrary, I would invite you to bet. I say that Acacia Clinics study design and analysis is correct and your study design and analysis is wrong. You say the opposite. Here are the rules for the bet. If you won’t bet, you are of course conceding that Acacia’s analysis is correct and your analysis, to use a technical biostatistical term, sucks.
I am already finding five rookie mistakes, and I’ve only read the first five pages.
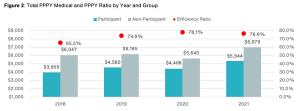
First take a looksee at this screenshot below. I was having a lot of trouble figuring out how the red dots showing something you’ve dubbed the “efficiency ratio” (a term which apparently has no meaning in health services research, as far as Google is concerned, while ChatGPT thinks it means something else altogether, but what do they know?) were related to the differences in the size of the bars. Then I realized you accidentally started the y-axis at $4000 instead of $0. A rookie mistake, which inadvertently makes the alleged savings look about 3 times higher than they are.
Meaning your so-called “efficiency ratio” is the value in the blue bar as a percentage of the gray bar, not the height of the blue bar as a percentage of the gray bar. Call me a traditionalist, but in my humble opinion those two ratios should be the same. (Note: apologies for the blurry screenshot. That’s how it’s reproducing.)
I did notice that later on, pretty much the same data in Figure 1 was reproduced as Figure 2, but this time you started the y-axis at $1000. So you’re definitely getting warmer!
Happy New Years!
Second, you may want to check your calendar, because it is now 2024. Your analysis ends at 2021. You’ve had almost two years and five full months plus a Leap Day to update it and yet, you cut it off in 2021. A cynic might conclude that you picked that end date because the alleged benefit you are claiming regresses further to the mean in 2022 and 2023.
Looks like you threw up in front of Dean Wormer
Third, speaking of regressing to the mean, the reason a cynic could infer that conclusion is, your so-called “efficiency ratio” already was regressing to the mean. Let’s assume, for now, the unassumable: that your “matched controls” are a legitimate study design. (If it were, the FDA would allow it.) Between 2018 and 2021, according to your own numbers on that chart, participant costs rose 31% while non-participant cost rose 22%. And yet somehow that statistic appears nowhere in your report, once again a rookie mistake.
Are you having connectivity issues?
Fourth, there are two types of outcomes researchers in our industry. Those who think “matched controls” are a valid study design for this kind of analysis, and those who have a connection to the internet. If you can’t afford my seminal book, try this article on the Validation Institute website which proves – using fifth-grade arithmetic – why that methodology doesn’t work. Period.
Perhaps the giveaway why “matched controls” don’t work in this case might be that the savings started on the first day of the baseline year. An employee has one phone call (yes, that was the cutoff point to get into the study group, though some people had many more) with one of Lyra’s “220,000 high-quality providers” and their medical spending drops precipitously. I’d also love to know what Lyra’s Secret Sauce is, that lets them retain 220,000 providers, all of whom are “high-quality.”
The following things change immediately as a result of that call, even though they are not part of the conversation and require a real doctor or in the case of ER visits, a great deal of luck:
- Non-mental health emergency visits plunge by 30%
- Generic drug scripts plunge by 30%
- By 2021, even expensive specialty meds fall by more than 20%
You might want to retain a smart person to explain the difference between correlation and causation. Alternatively, perhaps you are concerned that this meteor almost hit the visitors center?

A mystery wrapped inside a riddle wrapped inside a seven-figure consulting fee
Fifth, consider that Aon has data for:
- medical claims
- diagnoses
- professional mental health spending
- inpatient mental health spending
- outpatient mental health spending
- spending on non-mental health
- ED and inpatient visits
And consider that:
- They did this study for Lyra
- The study is called “Lyra Cost Efficiency [sic*] Results”
- The “Workforce Mental Health Program information was provided by Lyra Health”
Yet somehow – despite having the aforementioned two years, five months and a leap day to prepare this study – they claim to have absolutely no idea how much Lyra’s services cost:
We suspect it is a lot, perhaps enough that mental health professional fees with Lyra for participants exceed mental health spending by non-participants. Because in addition to having to pay their “evidence-based therapists” (Lyra’s term), sales, marketing, overhead and profit, Lyra needs to pay off the benefits consultants too, to “partner with” them:
Finally, where’s the guarantee of credibility? Does Aon not stand behind its work? I guess that’s a wise move on your part, because if you did, I’d be rich. By contrast, Acacia Clinics was validated by the Validation Institute (VI). They do stand behind their work, so the VI’s findings on Acacia Clinics’ outcomes are backed by a $100,000 Credility Guarantee. That, of course, is in addition to my own guarantee.
Did Mr. Ozminkowski just damage Lyra’s reputation…and Aon’s own?
The irony here is that Lyra is considered (or was considered, until this report) a perfectly legit vendor that is providing a valuable service of connecting employees to mental health professionals that match their needs. That is especially useful these days, when mental health benefits are very skinny and mental health providers are hard to come by. The “ROI” is employee appreciation, and possibly higher productivity. Not magical reductions in medical spending completely unrelated to the issues they are calling about.
Paying off consultants (who coincidentally also send them business) to pretend otherwise could damage that reputation. A rookie mistake on their part.
Further, there are some really smart, really honest consultants at Aon. But just like one dirty McDonalds would sully all of them, organization as a whole suffers when one consultant goes rogue.
*It’s either “efficiency,” meaning the cost vs. the benefit, or “cost-effectiveness.” “Cost efficiency” is redundant. They really shouldn’t need me to tell them that – or, for that matter, anything else in their report.
A lesson in valid measurement: Vida vs. Virta
The Peterson Health Technology Institute (PHTI) recently published an exhaustive study demonstrating what we’ve been saying (and guaranteeing) all along: Virta is unique among diabetes vendors in that it actually has an impact, while digital diabetes vendors don’t. (Diathrive, a diabetes supply company, also saves money but supplies are a different diabetes category.)
PHTI did a great job as far as the report went. And Livongo and Omada have accepted their conclusions. By “accepting their conclusions,” I mean declining my bet. Sure, they did some perfunctory whining about not looking at the data the right way yada yada yada in one of those “he said-she said” articles, but at this point everyone (at least everyone with a connection to the internet) knows they lose money.
That brings us to Vida. Until now Vida has flown under the radar screen, but the sound-alike name gives them the opportunity to be confused with Virta. That strategy was coupled with a brilliant two-part strategy regarding the PHTI report:
- Don’t submit any studies to PHTI
- Complain that PHTI didn’t look at their studies.
To the first point, PHTI lists cooperating vendors who submitted articles. (Virta submitted 12 to Vida’s 0.) To the second point, that aforementioned “he said-she said” article notes:
Vida says its diabetes programs are clinically proven to [reduce Hb A1c], as reflected in its body of peer-reviewed publications and the satisfaction of the “tens of thousands of members” who have found success with its diabetes program.
Not to be too semantic here on the latter point, but of course the people “who have found success” with your program will be satisfied. The question is what percentage have “found success.” In their case, according to this article, the percentage who dropped out or were lost to followup or didn’t complete their Hb a1c tests was…hmmm…I can’t seem to find it. Am I missing something here?
Results: Participants with HbA1c ≥ 8.0% at baseline (n=1023) demonstrated a decrease in HbA1c of -1.37 points between baseline (mean: 9.84, SD: 1.64) and follow-up (mean: 8.47, SD: 1.77, p<0.001) . Additionally, we observed a decrease in HbA1c of -1.94 points between baseline (mean: 10.77, SD: 1.48) and follow-up (mean: 8.83, SD: 1.94, p<0.001) among participants with HbA1c ≥ 9.0% (n = 618) .
Bookmark this paragraph because we will be coming back to it. Turns out one could teach an entire class based on this paragraph alone, comparing Vida to Virta. And Part 2 will do exactly that.
Peer Review
Here is the Validation Institute’s summary of so-called “peer-reviewed publications,” in Part 5 of their 9-part series on validity:
Vendors have realized that prospects consider the phrase “peer-reviewed” to settle all debates about legitimacy. Part Five will take you inside the thriving peer-reviewed journal industry to show you how peer reviews are bought and sold.
Often, vendors will brag about being peer-reviewed. Most prospects of vendors will then assume that the data was carefully vetted and reviewed by independent highly qualified third parties before seeing the light of publication because, after all, no journal would ever publish an article that was obviously flawed, right?
Well, certainly not for free.
Indeed, probably 95% of journals have turned article submission into a profit center. The euphemism for this business model is “open access.” Open access means that instead of the subscriber paying to read these journals, the author pays to publish in them. In other words, vendors are placing ads. Livongo at least had the good sense to at least pretend their journal was real, by buying some space in something called the Journal of Medical Economics, which sounds pretty legit, right? Not open-access, right? Um…
Well, Vida didn’t even bother to pretend it wasn’t open-access when they placed an ad (technically called “sponsored content”) in JMIR Formative Research. It actually includes the word “open” in the logo…
…and lest there be any doubt about where their vig comes from, JMIR even publishes their price list, which they call an “article processing fee.”
Also, have you ever heard the phrase “investigator bias“? Well, here is the list of authors and funders. Notice a pattern?
G. Zimmermann: Employee; Vida Health. A. Venkatesan: Employee; Vida Health. K. Rawlings: Employee; Vida Health. R. S. Frank: Employee; Vida Health. C. Edwards: Employee; Vida Health.
Vida Health
Like a real journalist, I reached out to Vida to ask for comments. Here’s what they wrote back:
- We aren’t submitting any comments
- But then we will complain that you didn’t look at our comments
Haha, good one, Al. Actually they didn’t say the second but wouldn’t it be funny if they do?
Official Rules for Diathrive $100,000 Challenge
Congratulations to Diathrive Health for achieving validation from the Validation Institute (VI). That itself comes with a $50,000 Credibility Guarantee.
In rare cases of VI-validated organizations – such as Virta Health or Sera Prognostics or Acacia Clinics – I add my own “Best in Show” guarantee and offer a $100,000 reward for a successful challenge.
Any diabetes vendor mentioned in the Peterson Health Technology Institute report (other than Virta, which “won” in that report for its diet/coaching offering, which is not at all competitive with Diathrive) can challenge my statement that Diathrive has better and more validly measured savings than they do on the cost of supplies from a vendor that also incliudes coaching support.
Rosencare, based on the industry-leading results at Rosen Hotels, has achieved excellent results overall with Diathrive, but the specific cash-on-cash savings that are guaranteed would be actual diabetic supply prices offered by a company that also provides coaching.
Here are the terms to earn the $100,000 reward.
Terms and Conditions of Challenge
Selection of Judges
There will be five judges, selected as follows:
- Each side gets to appoint one, drawn from members as of 4/17/24 of The Healthcare Hackers listserve with 1300 people on it, from all walks of healthcare.
- Two others are appointed objectively. That will be whichever health services researchers/health economists are the most influential at the time the reward is claimed. “Most influential” will be measured by a formula: the highest ratio of Twitter followers/Twitter following, with a minimum of 15,000 followers.
- Those four judges will agree on the fifth.
Using the criteria below, judging will be based on validity of the measurement. Measurements deemed invalid, such as those described on the Validation Institute site, are a disqualifying factor the challenger.
Written submissions
Each side submits up to 1000 words and five graphs, supported by as many as 10 links; the material linked must pre-date this posting to discourage either side from creating linked material specifically for this contest.
Publicly available materials from the lay media or blogs or the Validation Institute may be used, as well as from any academic journal that is not open-access.
Each party may separately cite previous invalidating mistakes made by the other party that might speak to the credibility of the other party. (There is no limit on those.)
If a challenger is “validated” by a third party whose alleged outcomes have been invalidated on this site in the past, those other invalidations may be presented to the judges to impeach the credibility of this alleged validation.
Oral arguments
The judges may rule solely on the basis of the written submissions. If not, the parties will convene online for a 2-hour recorded virtual presentation featuring 10-minute opening statements, in which as many as 10 slides are allowed. Time limits are:
- 30-minute cross-examinations with follow-up questions and no limitations on subject matter;
- 50 minutes in which judges control the agenda and may ask questions of either party based on either the oral or the written submissions;
- Five-minute closing statements.
Entry process
The entry process is:
- Challenger and TheySaidWhat deposit into escrow the amount each is at risk for ($10k for the Challenger, and $100k for TheySaidWhat). Each party forwards $10,000 to the judges as well, as an estimate of their combined fees and/or contributions to their designated nonprofits.
- If the Challenger or Service Provider pulls out after publicly announcing an application, the fee is three times the amount deposited.
- The escrow is distributed to the winner and the judges’ fees paid by the winner are returned by the judges to the winner, while the judges keep the losers’ fees.
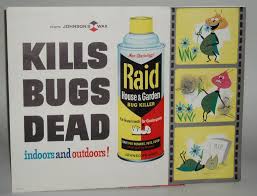
Peterson Center Kills the Diabetes Industry Dead
Last week the Peterson Health Technology Institute (PHTI, part of the Peterson Center on Healthcare) published the seminal report on the diabetes digital health industry, concluding that (with the clear exception of Virta, which we have also strongly endorsed) the minor health improvements claimed by Livongo, Omada and others nowhere near offset the substantial cost of these programs. To which we reply:
We, on the other hand, have known this since 2019. PHTI’s excuse, such as it is, is that it was formed in 2023. We’ll let it go this time…
The Likely Impact of the Findings
The report shows that digital health vendors (once again, with the exception of Virta, which emerged as the clear – and only – winner from this smackdown) are “not worth the cost.” We would strongly recommend reading it, or at least the summary in STATNews. It is quite comprehensive and the conclusion is well-supported by the evidence.
In the short run, the effect of this report should be Mercer renouncing its “strategic alliance” with Livongo (“revolutionizing the way we treat diabetes”) and returning the consulting fees it earned for recommending them to their paying clients. (Haha, good one, Al.)
This was a rookie mistake by Mercer in the first place. Not forming the “alliance,” but rather announcing it. The whole point of benefits consultants making side deals with vendors is to do it on the QT so clients don’t notice. Hence, I’m not saying Mercer should actually renounce Livongo and harm their business model. Just that they should pretend to.
In the long run, this report should signal the end of the digital diabetes industry, meaning Livongo, Omada, Vida and a couple I’ve never even heard of. The bottom line: private-sector employers using digital solutions for diabetes may be violating ERISA’s requirement that health programs benefit employees by being “properly administered.”
The Empire Better Not Fight Back
Inevitably, the well-funded diabetes industry will fight back against PHTI’s report and “challenge the data.” They’d be right in one respect: the data does need to be “challenged.” However, it’s for the opposite reason: PHTI went far too easy on these perps.
Here is what I would have added to the report, had they retained my services. (And I’d be less than honest if I didn’t admit I had hinted they should, but I think by then their budget was fully committed.) These points will inevitably come to light in the event of a “challenge.”
Second, matched controls are invalid because you can’t match state of mind. Ron Goetzel, the integrity-challenged leader of what Tom Emerick used to call the “Wellness Ignorati,” demonstrated that brilliantly, naturally by mistake. Take a looksee at what happens when you match would-be participants to non-participants – but without giving the former a program to participate in. The Incidental Economist piled on. And then the Wellness Ignorati tried to erase history, recognizing they had accidentally invalidated their entire business model. Diabetes is no different. There’s a reason the FDA doesn’t count studies that compare participants to non-participants, it turns out. PHTI accepted them as a control.
Third, along with sample bias there is investigator bias. Livongo’s main study was done by — get ready — Livongo. Along with some friends-and-relations from Eli Lilly and their consultants. PHTI assumed investigators were on the level. I’d direct them to Katherine Baicker’s two studies on the wellness industry. The first – whose “3.27-to-1 ROI” pretty much greenlit the wellness industry – was a meta-analysis of studies that were done – get ready – by the wellness industry. It has been cited 1545 times. The second, featuring Prof. Baicker’s own independently funded primary research, found exactly the opposite. It has been cited 16 times.
Don’t get us started on Livongo
Oops, make that a million and one.
Drawing undue attention to unwanted publicity has henceforth been termed The Streisand Effect. Right now this PHTI report is mostly of interest to the cognoscenti. Most of its customers won’t notice.
Why? Because what we say about wellness is likely also true here: “There are two kinds of people in the world. People who think diabetes digital health works, and people who have a connection to the internet.”
How Quizzify prevented another hospitalization – my own
For the second time in four years, Quizzify saved me a world of hurt. This time around was thanks to our Doctor Visit PrepKits, our companion app to Classic Quizzify, our healthcare trivia quizzes.
While the quizzes teach health literacy between clinical visits, the PrepKits teach health literacy specifically for clinical visits. You just enter a keyword, like a symptom, and the PrepKits tell you what you need to know, how to prepare for your visit, questions to ask the doctor and much more.
You might say “Well, our employees can just google on symptoms or ask their doctor.” Unfortunately, if I had just googled on “Swollen calf,” the first hit would be “no cause for concern.” (Try it.) And my doctor was quite convinced the PrepKits’ take on “swollen calf” was rather alarmist, but agreed to see me anyway.
Bottom line: Absent Quizzify2Go’s admittedly alarmist but nonetheless quite accurate advice that I should seek care urgently, I would have ended up in the hospital, with a procedure and a six-month recovery.
See how Quizzify once again saved the day…and turned a likely tale of woe into a minor inconvenience.
https://www.quizzify.com/post/how-quizzify-may-have-saved-my-life-again
And then imagine how many of your employees might have a similar experience. All you need is one, to pay for all of Quizzify.
PS Please put comments on Linkedin – I’ve migrated all the comments there.
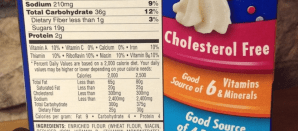
Those Nutrition Facts labels are, to use a technical term, crap.
There are precisely 3 pieces of useful information on these labels. Everything else ranges from useless to misleading.
And yet how often do you read those labels when selecting a product? And do you ever not believe the information on them? Well, it’s time to start reading these labels critically.
The food companies are “teaching to the test.” They are maximizing the perception that their products are healthy, instead of actually trying to create healthy products. Often the two goals are at odds with each other.
Please do not comment here. I’m taking all comments on Linkedin. This link takes you there, and then if you are still interested, you can link to the full blog post.
Oprah’s on Ozempic! Here’s how much that will cost you.
For better or worse, Oprah has been American’s biggest weight loss influencer since the liquid diet fad in the late 1980s. [SPOILER ALERT: That diet didn’t work.]
And now she’s all in for Ozempic. Of course, her regimen also includes significant exercise and presumably enough means to afford a healthy diet, but those nuances will likely be lost on your employees jumping on the GLP-1 bandwagon in hopes of a magic bullet.
Magic bullet or not, never before in the history of healthcare has anything – any drug, procedure, test, anything – combined this much effectiveness, popularity…and cost. Indeed, this single class of drugs will likely add 10 basis points to the overall US inflation rate in 2024. (You heard it here first, folks.)
Assuming you cover these drugs for weight loss, how you manage them will have a significant impact on not just your drug costs, not just your healthcare costs, but actually your entire compensation costs. In turn, private sector companies could feel a margin squeeze of about 1%, as this link shows.
You might say: “Well, we covered them in 2023 and costs didn’t go up that much.” Perhaps, but that was when these drugs were in shortage.
And also pre-Oprah. Holding back the weight loss drug coverage tide just got that much harder.
SPOILER ALERT: This is the ideal use case for Quizzify.